By Carolyn Brown
BS, MEd, RN, ARM, CWS, FACCWS
In Long Term Care, impaired skin integrity is an ongoing challenge. But now as residents are confined to their rooms due to COVID-19, those at risk for impaired skin integrity face even greater challenges.
Preventing pressure injuries while residents are confined to their rooms will require creative interventions. Today, our nationally recognized consultant, Carolyn Brown, helps address some timely caregiving questions related to immobility, nutrition and hydration.
Q: Immobility is a risk factor that places residents at risk for skin breakdown. Do you have suggestions for keeping our residents mobile while confined to their rooms?
A: Yes, that is absolutely correct – immobility is a risk factor that affects skin integrity. The less a resident moves, the greater their risk for developing a pressure injury. Here are a few suggestions you might initiate to keep residents active in their rooms:
- Focus on improving balance. Maintaining mobility relies heavily upon a steady balance. Residents have had fewer opportunities to walk and may become afraid of falling. To improve confident mobility, focus on improving balance with safety reminders, such as: “Mrs. Smith, your cane is right here to help you balance.”
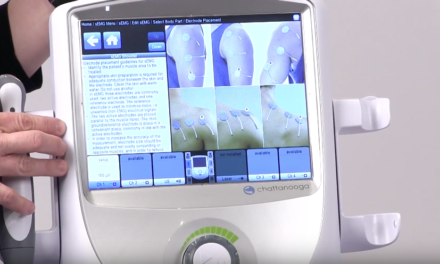
- Take advantage of product assistance. Another way you can help improve mobility may be through the use of walking aids. Whether your resident simply requires a cane, a walker or something in between, there are a variety of walking aids to help with mobility.
- Modify the living space. To improve mobility, it may be useful to rearrange the furniture, such as moving the bed and table to provide a better walking area. If possible, position a chair in front of the TV to encourage residents to get out of bed to watch their favorite programs.
- Consider the importance of having comfortable shoes that fit. During this prolonged isolation, residents’ feet and the fit of their shoes may have changed. To improve mobility, properly fitting and comfortable shoes will improve balance and confidence in ambulation. Also be certain that lower leg compression therapy continues to be properly sized and correctly applied.
Q: How can I encourage my residents to maintain adequate nutrition and hydration while they are dining in their rooms?
A: Undernutrition and dehydration are also risk factors for skin integrity. Adequate nutrition and healthy hydration are challenging in the dining room when caregivers can be close by to offer assistance. But when feeding residents in their rooms, there is a considerable possibility of weight loss and dehydration. I’ve heard of a few good ideas you may consider:
- Move the resident into their doorway for a fresh view of their community while eating. If both residents are up for meals, facing out of the window may also be an option to improve the appetite.
- Provide an opportunity for toileting and hand hygiene. Clean dentures, hearing aids and glasses to increase the dining experience.
- Offer a variety of food choices, especially their favorites.
- Offer snacks throughout the day – this can be an opportunity for safe, social interaction with residents, and always encourage a sip or two of their beverages.
- Assist residents during mealtimes according to their individual needs. While you’re in the room, observe for any functional changes.
A nurse I recently spoke with described a resident who ate independently in the dining room but was now unable to hold their fork. After a short discussion, it became evident that the resident’s arthritis pain had worsened. The nurse has since scheduled pain medication 45 minutes before meals. She is also assessing the benefit of adapted cutlery and eating aids to assist in eating independently.
- Review and revise the list of residents who require a supplement as appropriate.
- Prevent dehydration by proactively reassuring the resident that you will assist them to the toilet. As you know, residents may avoid fluids to prevent incontinent episodes. Drinks need to be within easy reach and a suitable cup provided.
- Offer fluids regularly throughout the day, and water should be fresh and to the resident’s preferred temperature.
About Carolyn
Carolyn Brown is a consultant to Direct Supply as well as a nurse educator, speaker and author with more than 35 years of operational experience in healthcare. She is a nationally recognized leader in supporting and helping post-acute care facilities thrive as they contend with tighter funding, new reimbursement methodologies and fewer resources.
From walking and eating aids to therapy solutions and more, you can find a huge selection of healthcare equipment for Senior Living at Direct Supply. Please contact us or call 1-866-300-4074 for product assistance. And be sure to visit our Insights page for more tips on helping maintain healthy skin.